For many years, new drug candidates have been tested out on animals, but in more recent years scientists have used in vitro models, where new drug candidates are tested on collections of human cells, organs and tumours that are laid out on petri dishes.
Testing new cell therapies for solid tumours like breast cancer comes with some unique challenges – these treatments often have side effects all over the body, some of which are tolerable and some of which are not, and the complexity of cell therapies means that the human body can sometimes respond in unexpected ways. Models need to be improved to reflect this.
At the moment, many in vitro models are focused on just one area of the body, one pathway or one interaction. This approach is perfect for examining a specific issue in detail, like whether a CAR-T cell treatment – a type of cell therapy that’s been very successful in certain types of cancers – is hitting the right targets, but it’s not ideal for predicting how the body will react to a new drug. Although the model developed by imSAVAR can’t exactly replicate how a human body will react, it can give researchers a better idea of how tissues will respond.
“Most in vitro models are focused on integrating only individual aspects. For instance, a model containing CAR-T cells together with a selection of tumour cells can tell you whether the CAR-T cell is specifically recognising the target tumour cells or if they are just killing any tumour cell they come into contact with,” says Peter Loskill, head of organ-on-chip research at the Eberhard Karls University Tübingen.
“However, if you want to look at how this will work overall in a patient and identify whether there are any additional safety aspects, you will miss them.”
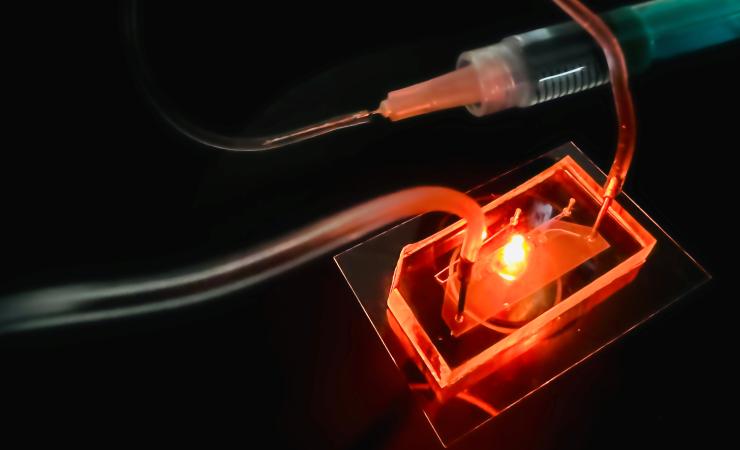
The IMSAVAR project set out to develop a breast-cancer-on-chip model that incorporates a suite of the body’s cells, giving a more realistic picture of how the body could respond to the cell therapies.
“If the CAR-T cells are really abundant compared to the tumour cells, they will release a lot of cytokines and that can induce toxicities,” explains Miriam Alb, a postdoc in the Hudecek Lab and the Fraunhofer IZI Branch on Cellular Immunotherapy at the University Hospital of Wurzburg, who leads imSAVAR’s work on immuno-oncology models. “The cytokines can recruit other immune cells from the bloodstream and other tissues and that can potentially trigger a vicious cycle.”
Endothelial cells, which line blood vessels and regulate the transfer of material between the bloodstream and surrounding vessels, play a big role in the recruitment of other immune cells and the multiplication of the cytokines. The endothelial cells can act as accelerants, speeding up the number of cells that the cytokines can recruit, which can build up and become life-threatening.
“In the standard assays, you won’t find these cells, so you won’t see these effects,” says Alb.
The new model developed by the imSAVAR project incorporates the effects of the endothelial cells, as well as other cells and tissues throughout the body, into a mix dubbed ‘the tumour microenvironment’. The new model is much better at predicting how a CAR-T cell treatment will affect the body as a whole, not just the tumour that it’s designed to attack.
“In the end, you need to find a balance for your drug that is sufficiently efficacious and not dangerous,” says Alb. “And if you can see that in one model, that is extremely valuable.”
Some features that the imSAVAR model boasts is the ability to test modulation approaches, like how much of a drug should be given and when. Combination therapies can also be tested on the new model, and more precise estimations of how to modulate and moderate risks can be obtained.
One feature that sets the imSAVAR model apart from the others is the ability to mimic the passage of fluid through the blood vessels over the course of eight days. Most other assays only run for 24 hours, meaning that researchers cannot monitor when the cytokines released or the drug that has been added leaves the system.
At a fork in the road
Going forwards, there are many next steps that the project could take. One option might be to add more complexity to the tumour microenvironment in the new model.
“There are other types of immune cells and stromal cells that also play a role in these complex mechanisms,” says Loskill. Integrating these cells into the model would improve the predictability of the model and make it even more similar to the human body response. The immune cells are particularly significant because – in solid tumours like breast cancer tumours – these cells can inhibit the progress of CAR-T therapies.
“Getting to the tumour is sometimes a struggle for CAR-T cells because of other cells and molecules in the microenvironment surrounding the tumour tissues, so looking into this and engineering the CAR-T cells so that they can survive this better is another step forward, and we could expand the models to test this,” says Alb.
Another approach would be to look at the combination of different types of organ-on-chip systems to get a more accurate glimpse at how the immune system can affect different parts of the body. Or the researchers could take a more personalised approach – because differences in individual patients can also be recreated in model systems which could deliver truly tailored treatments.
Directing research towards the end user
For the researchers, the benefit of working in a public-private collaborative project is that their results can be applied to real-life situations.
“The benefit of these public-private partnerships is that – from the beginning of this model’s development – the needs of the end users are taken into account and the direction is steered,” says Loskill.
According to Alb, the public-private framework has helped to overcome knowledge gaps, and the contributions of all the partners have smoothened the path towards better models – those that are better suited to reflecting the reactions of the human body to CAR-T cell therapy. This might help to also speed up clinical trials of newly developed cell therapies.
“There’s a translational gap from the classical in vitro assays to the in vivo animal models and then going into the clinical studies. This gap narrows down if you go into a consortium where people have different scientific backgrounds and different needs, and they’re coming together to work towards one goal,” says Alb.
imSAVAR is supported by the Innovative Medicines Initiative, a partnership between the European Union and the European pharmaceutical industry.